Views: 0 Author: Site Editor Publish Time: 2025-11-03 Origin: Site








Have you ever wondered how doctors explore the intricate pathways of your lungs? Bronchoscopy is the answer. It's a medical procedure using specialized instruments to examine the airways. In this post, you'll learn about the differences between rigid and flexible bronchoscopes. Understanding these differences is crucial for both patients and healthcare providers to ensure optimal care and outcomes.
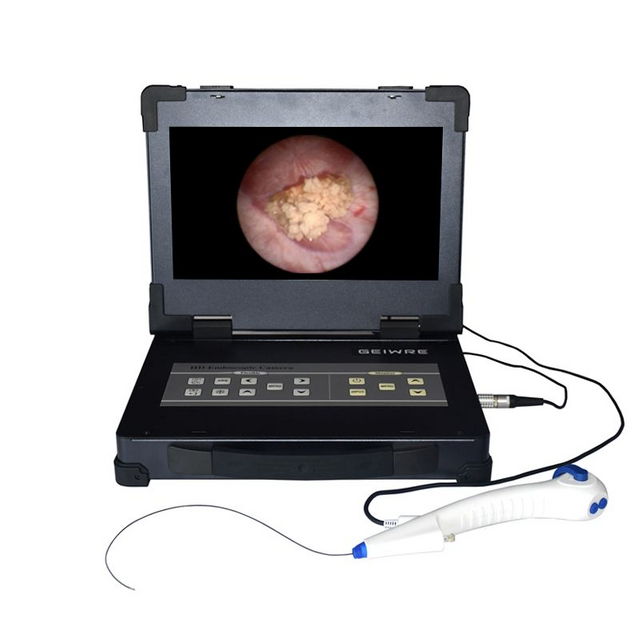
A flexible bronchoscope is a thin, tube-like instrument made from soft, bendable materials. It has a light source and a tiny camera at the tip, allowing doctors to see inside the airways. The flexibility lets it move easily through the nose or mouth, down the throat, and into the smaller branches of the lungs. Its diameter is small enough to pass through narrow airways, making it ideal for detailed inspection and sampling.
Inside the flexible bronchoscope, there is a channel for passing tools like biopsy forceps or suction devices. This design helps doctors collect tissue samples or remove mucus and foreign objects. The flexibility and small size make it comfortable for patients and suitable for outpatient procedures.
In contrast, a rigid bronchoscope is a straight, metal tube. It is larger and much less flexible than the flexible bronchoscope. The rigid bronchoscope is inserted through the mouth only, as its size and stiffness prevent nasal entry. Its wide diameter provides a larger working channel, enabling doctors to use bigger instruments during procedures.
The rigid bronchoscope is designed for stability and control, especially during complex interventions. It allows surgeons to maintain a clear airway and provide ventilation through the tube during surgery. Because of its size and rigidity, this instrument requires general anesthesia for patient comfort and safety.
| Feature | Flexible Bronchoscope | Rigid Bronchoscope |
|---|---|---|
| Material | Soft, bendable materials | Rigid metal |
| Diameter | Small, narrow | Larger, wide |
| Flexibility | Highly flexible, bends easily | Rigid, straight |
| Insertion Route | Nose or mouth | Mouth only |
| Working Channel Size | Small, for fine instruments | Large, for bigger tools |
| Patient Comfort | Usually local anesthesia or mild sedation | Requires general anesthesia |
| Usage | Diagnostic, minor therapeutic tasks | Complex therapeutic procedures |
The flexible bronchoscope’s design supports detailed exploration of the lung’s smaller airways. Its flexibility allows navigation through twists and turns, making it excellent for biopsy and minor treatments. On the other hand, the rigid bronchoscope’s solid structure provides better control during major interventions, such as removing large obstructions or controlling bleeding.
Each instrument’s design suits specific clinical needs. Understanding these differences helps healthcare providers choose the best bronchoscope for each patient and procedure.
Tip: When selecting a bronchoscope, consider the procedure's complexity and airway size to match the instrument's design capabilities for optimal patient outcomes.
Flexible bronchoscopes excel in their ability to bend and navigate through the complex pathways of the airways. Their thin, pliable design allows doctors to reach deep into the lungs, including the smaller and more twisted bronchial branches. This flexibility enables detailed inspection and targeted biopsy or suctioning in areas that rigid bronchoscopes cannot access. Because it can be inserted through the nose or mouth, it offers more options for patient comfort and procedure planning.
The flexible scope’s maneuverability also reduces the risk of trauma or injury to the airway walls. It can smoothly curve around sharp angles, making it ideal for diagnostic procedures or minor therapeutic tasks like removing small foreign bodies or clearing mucus plugs. Its design supports outpatient use, often requiring only local anesthesia or mild sedation, which improves patient tolerance and recovery time.
Rigid bronchoscopes, due to their solid, straight metal tube design, have limited flexibility and cannot navigate beyond the main airways. They must be inserted through the mouth, restricting access routes and potentially causing more discomfort. Because they cannot bend, they are less suited for exploring the smaller or more distal airways.
However, their rigidity provides excellent stability and control during procedures that require strong manipulation, such as removing large foreign bodies or controlling severe bleeding. The larger diameter allows for bigger instruments, but this comes at the cost of less maneuverability. The need for general anesthesia adds complexity to the procedure and may limit its use in patients who cannot tolerate such anesthesia.
The flexibility of the bronchoscope directly impacts the scope of procedures and patient outcomes. Flexible bronchoscopes are preferred for routine diagnostic exams and minor interventions because they can access more lung areas safely and comfortably. Their adaptability reduces procedure time and anesthesia risks.
Rigid bronchoscopes remain critical for complex therapeutic cases where control and a wide working channel are essential. For example, they are ideal for removing large airway obstructions or managing massive bleeding, where precision and airway security are paramount.
Understanding these differences helps clinicians select the most appropriate bronchoscope based on the patient’s condition, airway anatomy, and procedure goals.
Flexible bronchoscopy usually requires only local anesthesia combined with mild sedation. Doctors often spray a numbing agent into the nose or throat to reduce discomfort as the thin, flexible tube passes through. Sedatives help patients relax and minimize anxiety during the procedure. This approach allows patients to remain awake but comfortable, making it suitable for outpatient settings. The lighter anesthesia also means quicker recovery times and fewer risks compared to general anesthesia.
Rigid bronchoscopy demands general anesthesia because the rigid metal tube is larger and less forgiving. Patients are fully unconscious to ensure comfort and safety. General anesthesia prevents gagging, coughing, or movement that could cause injury during insertion and manipulation of the rigid scope. It also allows doctors to maintain airway control and ventilation through the bronchoscope during complex procedures. Because general anesthesia carries higher risks and requires specialized monitoring, rigid bronchoscopy typically takes place in an operating room with an anesthesiologist present.
Patients tolerate flexible bronchoscopy better due to the less invasive nature and lighter anesthesia. They usually experience minimal throat soreness and can resume normal activities sooner. In contrast, rigid bronchoscopy can cause more throat discomfort and requires longer recovery due to the size of the instrument and the effects of general anesthesia. However, rigid bronchoscopy’s anesthesia approach is necessary for safety during more invasive interventions.
The choice of anesthesia reflects the bronchoscope type and procedure complexity. Flexible bronchoscopy’s sedation supports quick diagnostics and minor treatments, while rigid bronchoscopy’s general anesthesia suits major therapeutic procedures requiring full airway control.
Flexible bronchoscopes are the go-to tool for many diagnostic procedures. Their slim, bendable design allows doctors to explore the tiniest and most complex parts of the lungs. They can reach deep into the smaller airways, making it easier to collect tissue samples or secretions for lab analysis. This helps diagnose infections, lung tumors, or other lung diseases. For example, if a chest scan shows an abnormal spot, a flexible bronchoscope can be used to perform a biopsy, helping determine if it's cancer or another condition. Its ability to navigate around twists and turns means less discomfort for patients and quicker procedures.
Rigid bronchoscopes are mainly used for more invasive, therapeutic procedures. Their larger size and sturdy structure allow doctors to perform tasks that flexible scopes can't handle. For instance, removing large foreign objects lodged in the airway, controlling severe bleeding, or dilating narrowed airways are typical uses. The rigid scope’s bigger working channel also permits the use of larger instruments, making it ideal for complex interventions. Because of its size, this procedure requires general anesthesia and is usually performed in an operating room. Rigid bronchoscopy provides excellent control and visibility, crucial during life-saving or major airway procedures.
Selecting between a flexible and a rigid bronchoscope depends on the specific clinical situation. For most diagnostic tests, flexible bronchoscopes are preferred due to their minimally invasive nature and ability to access small, distal airways. They are suitable for outpatient settings, often under local anesthesia or mild sedation. Conversely, when the procedure involves removing large obstructions, managing significant bleeding, or performing extensive repairs, rigid bronchoscopes are better suited. Their stability and capacity for bigger instruments make them the tool of choice for complex therapeutic interventions.
Healthcare providers evaluate factors like airway size, the nature of the problem, and the complexity of the intervention before choosing the appropriate scope. Sometimes, both types are used together during a procedure to maximize safety and effectiveness. Understanding these differences ensures the right tool is used, improving patient outcomes and reducing risks.
Flexible bronchoscopy is the most common type used worldwide. Its versatility, minimally invasive nature, and outpatient feasibility make it a go-to choice for many healthcare providers. Hospitals and clinics perform it regularly for diagnostic and minor therapeutic tasks. Its widespread availability stems from its ease of use, lower cost, and safety profile. Many medical centers have dedicated bronchoscopic units equipped with flexible scopes, allowing quick access for routine procedures like biopsies, mucus removal, or airway inspection. This high prevalence ensures that most patients needing airway evaluation can receive the procedure without extensive delays or specialized centers.
Rigid bronchoscopy, in contrast, remains a specialized tool reserved for complex or emergency cases. Its use is limited to hospitals with trained thoracic surgeons and anesthesiologists experienced in this technique. Rigid scopes are often found in tertiary care centers, academic hospitals, or specialized thoracic surgery units. They are critical for procedures that require larger instruments, such as removing large foreign bodies, controlling significant bleeding, or performing airway dilations. Because rigid bronchoscopy demands general anesthesia and more complex setup, its availability is lower than flexible bronchoscopy. Nonetheless, for specific indications, it remains indispensable, especially in life-threatening situations.
Choosing between flexible and rigid bronchoscopy depends on multiple factors. The patient's condition, airway anatomy, and the procedure's complexity all play roles. For routine diagnostics, outpatient settings, or minor interventions, flexible bronchoscopy is preferred due to its safety, comfort, and accessibility. Its ability to navigate small, twisted airways makes it ideal for sampling and inspection. Conversely, when the intervention involves large obstructions, significant bleeding, or complex repairs, rigid bronchoscopy offers better control and larger working channels. Availability of trained personnel and equipment also influence decision-making. Some centers may lack rigid scopes or the expertise to use them, limiting their use to specialized facilities. Ultimately, the clinical scenario, resource availability, and patient safety guide the choice.
Before any bronchoscopy, thorough preparation is essential to ensure safety and success. Your healthcare team will review your medical history, current medications, and any previous issues with anesthesia or airway management. Inform your doctor about:
Neck or head problems, such as stiffness or limited movement
Dental issues, especially loose teeth or non-fixed dental prostheses, which should be removed before the procedure
Past surgeries or radiation on the head or neck area
Conditions like rheumatoid arthritis that may affect joint mobility
Use of blood thinners or antiplatelet drugs, which may need to be paused before the procedure
Any difficulties with intubation during past surgeries
This information helps the team anticipate challenges and plan the anesthesia and procedure accordingly. Your doctor may order blood tests, chest X-rays, or other exams to assess your overall health. Medication adjustments might be necessary to reduce bleeding risk or manage other conditions.
On the day of the procedure, fasting is usually required—no food or drink after midnight. This reduces the risk of aspiration during anesthesia. You should arrange for someone to drive you home afterward, especially if sedation or general anesthesia is used.
For flexible bronchoscopy, local anesthesia and mild sedation are common, so outpatient preparation suffices. Rigid bronchoscopy requires general anesthesia, often performed in an operating room, with more extensive monitoring and support.
Before the procedure, the medical team will explain what to expect and answer your questions. They will also check vital signs and place an intravenous line for medication administration.
Bronchoscopy is generally safe but carries some risks. Your care team will monitor oxygen levels, heart rate, and blood pressure throughout. They will ensure airway security, especially during rigid bronchoscopy, where airway control is critical.
Potential complications include bleeding, infection, or airway injury. These risks are minimized by careful patient selection, preparation, and skilled technique. After the procedure, you will be observed until anesthesia effects wear off and swallowing reflex returns to prevent aspiration.
If you experience symptoms like persistent coughing, severe throat pain, fever, or coughing up blood, notify your doctor immediately.
Flexible bronchoscopes are bendable and ideal for diagnostic tasks, while rigid bronchoscopes offer stability for complex interventions. Patients benefit from quicker recovery with flexible scopes, whereas rigid scopes provide control during major procedures. Healthcare providers must choose based on procedure complexity and patient needs. As bronchoscopy advances, Hengjia's products continue to offer innovative solutions, ensuring improved patient outcomes and procedural efficiency.
A: A Flexible Bronchoscope is a thin, bendable instrument with a camera and light, allowing doctors to inspect and navigate the airways easily.
A: Flexible Bronchoscopes are used for diagnostic procedures, such as biopsies and mucus removal, due to their ability to access small and twisted airways.
A: Flexible Bronchoscopes offer more comfort and access to smaller airways, making them ideal for routine diagnostics and minor interventions.
A: Flexible Bronchoscopes generally have lower costs associated with outpatient procedures, local anesthesia, and minimal recovery time.
A: Flexible Bronchoscopes provide detailed lung inspections, reduced trauma risk, and better patient comfort, enhancing diagnostic accuracy and patient outcomes.
